Pediatric cancer recurrence prediction has taken a significant leap forward with the advent of advanced AI technologies. A recent Harvard study highlights how this innovative approach outstrips traditional methods in evaluating the relapse risk in young cancer patients, particularly those suffering from gliomas. By leveraging multiple MRI scans over time, the AI tool not only enhances MRI scan accuracy but also optimizes patient care during a critical treatment period. With trends toward integrating AI in pediatric oncology, there’s hope for more tailored pediatric glioma treatment options that minimize the psychological burden on these young patients. As the research expands, the potential for using temporal learning AI to inform clinical decisions represents a transformative step in how we tackle pediatric cancer recurrence.
The challenge of forecasting cancer resurgence in children, especially in relation to brain tumors, has sparked interest in cutting-edge predictive models. Recurrence forecasting in young oncology patients is crucial for effective treatment plans and highlights the need for sophisticated tools that can analyze patient data longitudinally. With emerging techniques that assess glioma relapse risk through a series of imaging studies, medical professionals are beginning to embrace a new era of AI-backed diagnostics. This fresh perspective on pediatric oncology, emphasizing continuous monitoring via MRI scans, aims to alleviate some of the stress associated with routine follow-ups. Indeed, integrating these advanced predictive insights could reshape strategies for managing pediatric glioma treatment.
Understanding AI’s Role in Pediatric Oncology
Artificial Intelligence (AI) is revolutionizing pediatric oncology by providing advanced tools that significantly enhance the accuracy of diagnosing and predicting treatment outcomes. Traditional methods often rely on historical data and limited imaging, which can lead to inaccuracies in patient assessments. In contrast, AI in pediatric oncology leverages vast datasets and sophisticated algorithms to analyze patterns that human eyes might miss, enabling more tailored treatment plans. The integration of AI tools allows clinicians to focus on personalized approaches, enhancing the quality of care for children diagnosed with cancer.
The implementation of AI technologies also extends to various forms of diagnostic imaging, which aids in early detection and continuous monitoring of pediatric cancers. By utilizing data from MRI scans and other imaging modalities, AI can create a comprehensive picture of a patient’s health status over time. This ongoing evaluation is particularly crucial for conditions like gliomas, where the risk of recurrence can vary drastically. As AI continues to develop, its potential applications in pediatric oncology will undoubtedly expand, offering families hope for better outcomes.
Predicting Pediatric Cancer Recurrence Risk
The challenge of predicting pediatric cancer recurrence has long hindered effective post-treatment care. However, a recent study showcased how AI tooling, particularly through temporal learning AI, has outperformed traditional methodologies in assessing the risk of relapse in pediatric patients with gliomas. By analyzing a series of MRI scans over a specified period, researchers were able to discern patterns that indicated a higher likelihood of recurrence, providing a more precise prognosis that could guide future treatment protocols.
This advanced prediction capability offers valuable insights into patient management, potentially reducing the emotional and physical burden on families. By identifying high-risk patients, clinicians can strategize early interventions, including the possibility of prophylactic therapies to stave off relapse. This predictive approach not only prioritizes patient safety but also optimizes resource allocation within healthcare settings, underscoring the critical role of AI in transforming pediatric oncology care.
The Impact of MRI Scan Accuracy on Treatment Outcomes
MRI scans are fundamental in the diagnosis and monitoring of pediatric tumors. However, the accuracy of these scans is often influenced by several factors, including the interpretation of imaging and the technology used. Recent advancements in MRI techniques, particularly through AI integration, have significantly improved image quality and diagnostic precision. For instance, AI tools are adept at identifying subtle abnormalities in scan images that may suggest early signs of recurrence in gliomas, thereby enhancing treatment outcomes for pediatric patients.
Higher accuracy in MRI scans not only assists in better diagnosis but also plays a crucial role in patient comfort by minimizing the number of unnecessary scans. With AI’s capability to detect changes in a patient’s condition over time, there may be potential to streamline patient follow-ups, focusing resources on those who need it most. This evolution in diagnostic accuracy ultimately fosters a more efficient and compassionate approach to pediatric cancer management.
Temporal Learning AI: A Game Changer in Cancer Prediction
The emergence of temporal learning AI represents a significant advancement in predicting cancer recurrence. Unlike traditional models that often rely on individual images, temporal learning utilizes a sequence of MRI scans to provide insights into changes over time. This method effectively captures the evolution of gliomas, enabling clinicians to assess the progression of the disease dynamically. Research has shown that using multiple scans dramatically increases prediction accuracy, turning a previously static approach into a proactive one.
Temporal learning AI’s ability to synthesize data over an extended period allows healthcare providers to implement timely interventions based on predictive insights. For pediatric patients, this means not only a higher likelihood of catching recurrences early but also the potential to tailor follow-up treatments more effectively. As this technology continues to advance, it paves the way for innovative strategies in the management and treatment of pediatric cancers, ensuring better patient outcomes.
The Future of Pediatric Glioma Treatment
As research progresses, the future of pediatric glioma treatment is becoming increasingly optimistic thanks to advancements in technology and techniques like AI. The integration of AI tools in clinical settings has the potential to personalize treatment plans based on individual patient data derived from comprehensive imaging analyses. This shift towards precision medicine helps in tailoring therapies that cater specifically to characteristics of the tumor, leading to improved success rates for children battling gliomas.
Besides improved outcomes, AI also holds promise for reducing the side effects associated with aggressive treatment modalities. By precisely mapping out the extent and behavior of tumors, clinicians can create more effective yet less toxic treatment regimes. This approach could contribute significantly to enhanced quality of life for pediatric patients and their families, highlighting the importance of ongoing innovation in pediatric oncology.
The Importance of Clinical Trials in AI Development
As research into AI’s applications in pediatric oncology progresses, clinical trials play a pivotal role in validating these innovative tools within real-world settings. These trials provide essential data on the efficacy and safety of AI-based predictions for pediatric cancer, particularly in accurately forecasting glioma relapse risk. Through systematic evaluation, researchers can identify best practices that will streamline the integration of AI tools into everyday clinical protocols.
Furthermore, clinical trials serve as platforms for collaboration among multidisciplinary teams, including oncologists, data scientists, and radiologists. This collaborative effort is vital in developing comprehensive approaches that consider the complexities of pediatric cancer management. As trials yield positive results, they pave the way for broader adoption of AI technologies, ultimately revolutionizing the landscape of pediatric oncology treatment and care.
Addressing Family Concerns and Emotional Stress
Families dealing with pediatric cancer are often thrust into a whirlwind of uncertainty and stress. The prospect of cancer recurrence can weigh heavily on both patients and their families. AI tools that predict pediatric cancer recurrence can significantly alleviate some of these fears by providing clearer insights into a child’s health trajectory. Understanding potential relapse risks enables families to prepare more effectively for future interventions, ensuring they are not caught off-guard should the need for further treatment arise.
Being informed about the specific risks associated with a child’s glioma allows families to better engage with healthcare providers in decision-making processes. This partnership fosters confidence in the care plan and can mitigate feelings of helplessness often associated with cancer treatment. As AI continues to provide predictive insights, it delivers not just clinical data, but also a comforting sense of control to families navigating the complexities of pediatric oncology.
Reducing the Burden of Frequent Follow-Ups
In traditional pediatric oncology care, frequent MRI scans are necessary to monitor for potential recurrences. This continual testing can be taxing, both emotionally and physically, for children and their families. However, the advent of AI-driven prediction models changes this paradigm significantly. By harnessing temporal learning AI to analyze existing scans, healthcare providers may soon be able to minimize the frequency of these follow-ups for low-risk patients, thereby reducing unnecessary stress and exposure to medical environments.
This shift not only brings relief to families but also allows for a more efficient allocation of medical resources. By focusing attention on high-risk patients who require close monitoring, clinicians can ensure that the most vulnerable children receive the care they need. Consequently, the overall healthcare experience becomes more streamlined, allowing families to focus their energy on recovery and wellness rather than constant anxiety over upcoming appointments.
The Collaborative Efforts in Pediatric Cancer Research
Collaboration is essential in the realm of pediatric cancer research, as seen in studies involving multiple institutions like Mass General Brigham and Boston Children’s Hospital. Such partnerships facilitate the pooling of resources, expertise, and data necessary for groundbreaking advancements such as those pertaining to AI’s role in predicting pediatric cancer recurrence. By uniting professionals from various disciplines—oncology, radiology, and artificial intelligence—researchers can effectively tackle complex problems and accelerate discoveries that benefit young patients.
These collaborative efforts lead to a richer understanding of gliomas and enhance predictive capabilities through more comprehensive datasets. With nearly 4,000 MRI scans analyzed in a recent study, the findings underscore the power of teamwork in medical research. As institutions coalesce to present unified studies, the future of pediatric oncology looks brighter, promising innovative solutions to meet the unique challenges faced by children with cancer.
Frequently Asked Questions
How does AI enhance pediatric cancer recurrence prediction for gliomas?
AI enhances pediatric cancer recurrence prediction for gliomas by analyzing multiple MRI scans over time, utilizing a method known as temporal learning. This approach allows the AI to detect subtle changes across sequential scans and predict the likelihood of relapse with improved accuracy, significantly outperforming traditional single-scan methods.
What is temporal learning AI and its role in predicting glioma relapse risk?
Temporal learning AI is a technique that organizes and analyzes a patient’s MRI scans chronologically to identify patterns of change over time. This method has been shown to significantly increase the accuracy of predicting glioma relapse risk, as it captures the evolving nature of the tumor better than analyzing individual scans alone.
What improvements have been made in MRI scan accuracy for pediatric glioma treatment?
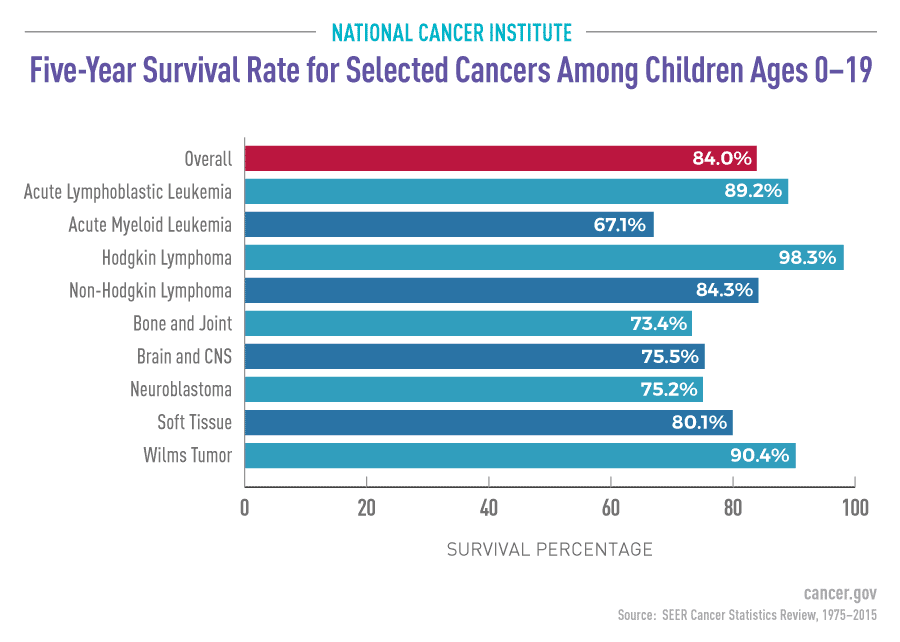
With the integration of AI and temporal learning, MRI scan accuracy in predicting pediatric glioma treatment outcomes has improved dramatically. The AI model can predict relapse risk with an accuracy range of 75-89%, a remarkable enhancement over the previous 50% accuracy based solely on single image analysis.
What challenges do pediatric oncology professionals face in predicting cancer recurrence?
Pediatric oncology professionals face challenges in identifying which patients are at highest risk for cancer recurrence, particularly for conditions like gliomas. This uncertainty leads to prolonged and stressful follow-up care, involving frequent MRI scans. Improved predictive tools like those utilizing AI aim to mitigate these challenges.
How does the AI tool predict pediatric cancer recurrence compared to traditional methods?
The AI tool predicts pediatric cancer recurrence more effectively than traditional methods by analyzing continuous data from multiple MRI scans rather than a single instance. This approach allows for a more comprehensive understanding of tumor behavior and early detection of potential relapse.
What are the implications of AI in pediatric oncology for glioma treatment strategies?
The implications of AI in pediatric oncology are significant, as it can help tailor glioma treatment strategies by accurately identifying patients at high risk for recurrence. This could lead to more personalized treatment plans, potentially allowing low-risk patients to receive less intensive monitoring while allocating more resources to high-risk cases.
What future developments are expected in AI-driven pediatric cancer recurrence prediction?
Future developments in AI-driven pediatric cancer recurrence prediction may include the initiation of clinical trials to validate current findings and further refine predictive models. Researchers anticipate that advancements in AI could contribute to more effective monitoring protocols and therapeutic strategies for pediatric glioma patients.
What is the significance of the study published in The New England Journal of Medicine AI regarding pediatric cancer recurrence?
The study published in The New England Journal of Medicine AI is significant as it reveals that AI tools can surpass traditional methods in predicting pediatric cancer recurrence, specifically in gliomas. This breakthrough research highlights the potential of AI to revolutionize patient care by improving risk assessment and management in pediatric oncology.
| Key Point | Detail |
|---|---|
| AI Tool Development | A new AI tool trained to analyze multiple brain scans significantly outperforms traditional methods in predicting relapse risk in pediatric cancer patients. |
| Study Insights | The study revealed that the AI’s temporal learning model can predict recurrence of both low- and high-grade gliomas one year post-treatment with accuracy ranging from 75% to 89%. |
| Research Collaboration | Conducted by Mass General Brigham in collaboration with Boston Children’s Hospital and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. |
| Clinical Application | The model aims to enhance patient care by potentially reducing follow-up imaging for low-risk patients and identifying high-risk patients for proactive treatment. |
| Future Directions | Further validation is needed in clinical settings, with plans to initiate clinical trials to evaluate AI-generated risk predictions. |
Summary
Pediatric cancer recurrence prediction has greatly advanced with the introduction of an AI tool that significantly surpasses traditional methods in relapse risk forecasting. This innovative approach leverages temporal learning to analyze brain scans over time, providing better insights into the likelihood of cancer recurrence in pediatric patients with gliomas. By increasing prediction accuracy and improving patient care, this study marks a pivotal step forward in the treatment of pediatric brain tumors, ensuring that healthcare strategies can be more accurately tailored to each child’s unique medical needs.