Alzheimer’s research stands at the forefront of understanding neurodegenerative diseases, particularly as scientists uncover the vital role of microglial cells within the brain’s immune system. These specialized cells are crucial for maintaining brain health by clearing away damaged cells and sculpting neural connections, yet their malfunction can lead to devastating disorders, including Alzheimer’s disease. Pioneering work by Beth Stevens and her team at Boston Children’s Hospital has revealed that improper pruning by microglia may contribute significantly to the disease’s progression. This groundbreaking research not only offers new avenues for treatment for Alzheimer’s but aims to identify biomarkers that could enable early detection of such illnesses. As the prevalence of Alzheimer’s continues to rise among the aging population, the implications of such findings are more critical than ever, with potential impacts on millions of individuals and families affected by this relentless illness.
In the realm of cognitive health, investigations into Alzheimer’s offer a promising glimpse into the complexities of neurodegenerative conditions. The innovative studies highlight the importance of the brain’s protective mechanisms, particularly focusing on immune cells known as microglia, which have been shown to influence neuronal health and functionality. Research spearheaded by prominent scientists like Beth Stevens has provided critical insights into how these cells may contribute to the onset of Alzheimer’s through their pruning activities. Advancements in this field are paving the way for novel therapies targeting these pathways, creating hope for more effective management and early intervention in cognitive decline. As the scientific community embraces these discoveries, they herald a new era in the fight against dementia and other related disorders.
Understanding Microglial Cells in Alzheimer’s Research
Microglial cells are essential components of the brain’s immune system, and their role in Alzheimer’s research has garnered significant attention in recent years. These cells monitor the brain for signs of damage or disease, actively participating in the removal of dead neurons and maintaining synaptic health. Their function is particularly crucial in recognizing aberrant conditions, which can contribute to neurodegenerative diseases such as Alzheimer’s. Researchers like Beth Stevens have illuminated how dysfunctional microglial activity can lead to excessive pruning of synapses, potentially exacerbating Alzheimer’s symptoms.
The transformative research conducted by Beth Stevens and her team at Boston Children’s Hospital and the Broad Institute has provided vital insights into how microglial cells interact with neurons. It has been observed that when microglia malfunction, they may not adequately support synaptic stability, leading to cognitive decline. By understanding these mechanisms, scientists can better inform treatment strategies and identify biomarkers for early detection of Alzheimer’s, ultimately impacting the lives of millions of patients suffering from neurodegenerative disorders.
The Role of the Brain’s Immune System in Neurodegenerative Diseases
The brain’s immune system, primarily comprised of microglial cells, plays a critical role in maintaining neuronal health and function. This immune response is crucial in neurodegenerative diseases, where the usual protective restoration processes can become dysregulated. In the context of Alzheimer’s disease, microglial dysfunction can result in neuroinflammation, contributing to the pathology of the disease. Revealing how microglial cells protect against or contribute to neurodegenerative diseases is fundamental for developing therapies that could bolster the brain’s immune response.
Researchers aim to enhance our understanding of the balance between healthy microglial activity and maladaptive responses that lead to neurodegeneration. Investigations into this delicate equilibrium can aid in pinpointing new therapeutic targets. For instance, fostering a more efficient microglial response might help in early intervention strategies for neurodegenerative diseases, including Alzheimer’s. The potential benefits significantly underline why ongoing research in microglial cells remains a dynamic and crucial field.
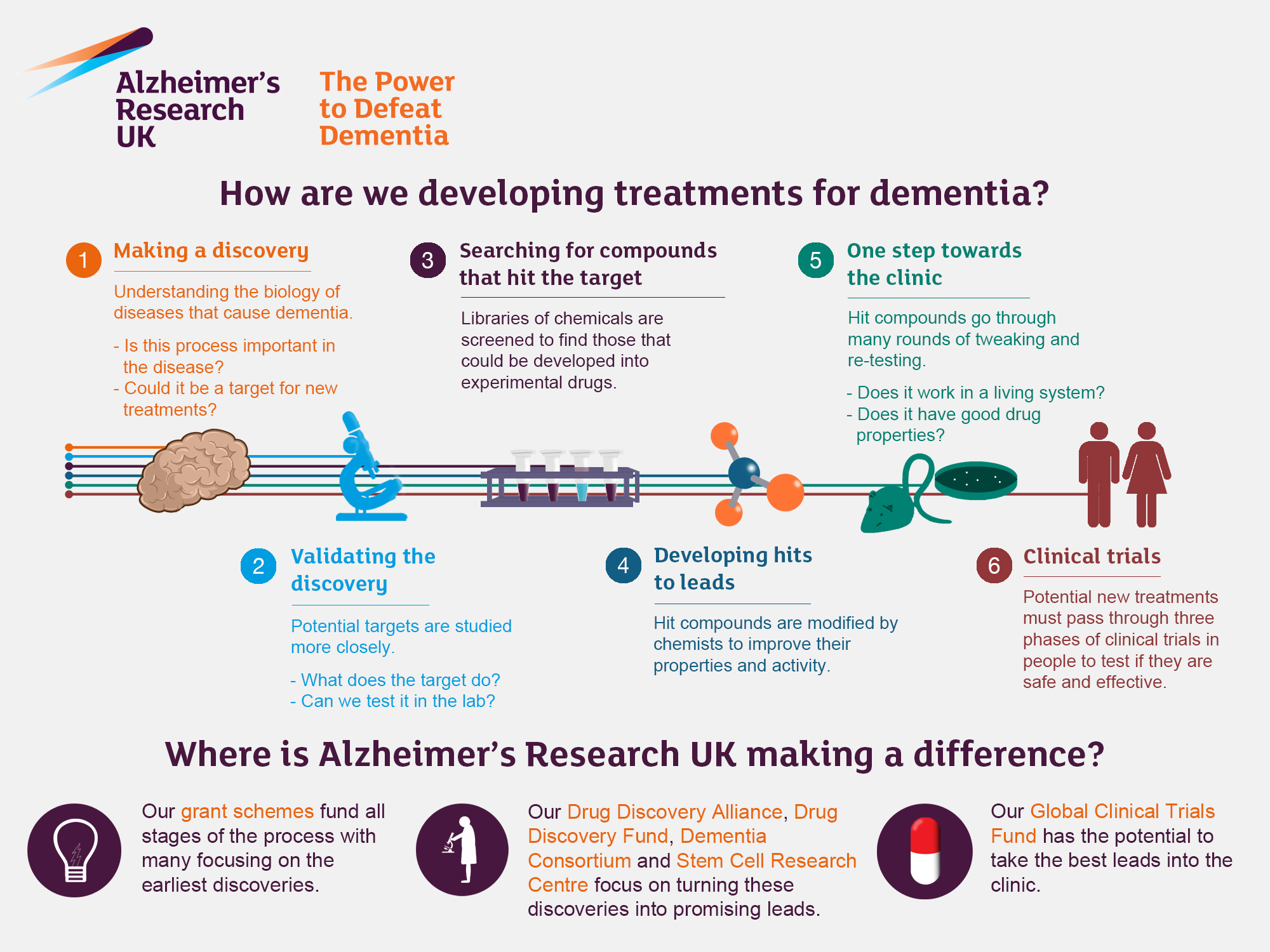
Innovative Treatments for Alzheimer’s Disease
With the rising number of Alzheimer’s cases, innovative treatment approaches are essential to manage this growing health crisis. Recent advancements in understanding microglial biology have opened new avenues for therapeutic interventions. Researchers like Beth Stevens are investigating how modifying microglial activity might result in more effective treatments for Alzheimer’s. This includes designing drugs that target the pathways by which microglia contribute to synaptic pruning and neuroinflammation.
Promising research has resulted in potential treatment strategies, such as pharmacological agents that can manipulate microglial functions to reduce neuroinflammation. These innovations not only aim to slow the progression of Alzheimer’s but also strive to remediate some of the cognitive deficits associated with the disease. As the scientific community advances in understanding the underpinnings of Alzheimer’s pathology, novel therapies continue to evolve, paving the way for a better quality of life for those affected.
Beth Stevens: Pioneering Alzheimer’s Research
Beth Stevens stands out as a pioneering neuroscientist whose work has had substantial implications for Alzheimer’s research. Her investigations into microglial activity have transformed how scientists perceive the brain’s immune system and its role in neurodegenerative diseases. By following her scientific curiosity, Stevens has unveiled critical insights into the mechanisms of synaptic pruning and how their dysfunction can lead to diseases like Alzheimer’s. Her recognition as a MacArthur ‘genius’ highlights the significance of her contributions to neuroscience.
In addition to her groundbreaking research, Stevens emphasizes the importance of federal funding in advancing Alzheimer’s research. The support from institutions like the National Institutes of Health has allowed her lab to explore the foundational aspects of microglial biology, paving the way for future discoveries. Through her ongoing commitment to investigating the links between microglia and cognitive diseases, Stevens continuously influences the trajectory of treatments and interventions aimed at combating Alzheimer’s.
The Future of Alzheimer’s Research
Looking ahead, the future of Alzheimer’s research is promising, with emerging studies focusing on the role of the immune system in brain health. As understanding deepens around microglial cells and their functional roles, researchers can develop better diagnostic tools and treatment methodologies. The ongoing work of scientists like Beth Stevens is crucial for informing these developments. With advancements in technology and interdisciplinary collaborations, Alzheimer’s research is entering a new era of innovation.
Moreover, the integration of genetics and neuroimaging techniques will play a critical role in unraveling the complexities of Alzheimer’s disease. Future studies may uncover specific genetic markers associated with microglial dysfunction and neuroinflammation, leading to targeted therapies. As the scientific community rallies around this focus, the combined efforts may significantly improve the detection and management of Alzheimer’s, fostering hope for millions at risk of developing this debilitating disease.
The Importance of Early Detection in Alzheimer’s
Early detection of Alzheimer’s disease is essential for effective intervention and management of the condition. With innovative research into biomarkers and microglial activity, scientists are making strides in identifying signs of Alzheimer’s long before cognitive decline becomes evident. By focusing on the changes in microglial functions, researchers can establish critical windows of opportunity for treatment that may alter the disease’s trajectory.
As evidenced by the research led by Beth Stevens, recognizing the role of the brain’s immune system opens new pathways for early diagnosis. This proactive approach can enhance patient outcomes, providing individuals and their families with the necessary resources and support as the disease progresses. By fostering public awareness about the importance of early detection and the ongoing research efforts, we can advocate for improved strategies in combating Alzheimer’s.
Challenges in Treating Neurodegenerative Diseases
Treating neurodegenerative diseases, particularly Alzheimer’s, presents numerous challenges. One of the foremost issues is the variability in individual responses to available treatments, which can be partly attributed to the complexity of neurodegenerative pathology. The malfunctions of microglial cells and the resultant neuroinflammation represent just a fraction of the overall disease mechanisms, suggesting that a multi-faceted treatment approach is necessary to address the various dimensions of Alzheimer’s.
Furthermore, the stigma often associated with Alzheimer’s can hinder access to timely medical interventions. Initiatives designed to mitigate these barriers are crucial, as they can empower individuals at risk of developing neurodegenerative diseases to seek early diagnosis and treatment. Ongoing research led by dedicated scientists like Stevens aims to bridge the existing gaps in understanding and treatment, ultimately providing hope amidst the challenges faced.
The Intersection of Basic Science and Clinical Applications
The interplay between basic science and clinical applications is crucial in advancing Alzheimer’s research. The foundational studies examining microglial cells not only unravel complex biological mechanisms but also lay the groundwork for developing therapeutic interventions. The research conducted by Beth Stevens exemplifies how curiosity-driven science can lead to profound clinical implications, creating a pathway from hypothesis to real-world application.
As scientists meticulously study the relationship between neuroinflammation and cognitive decline, they gather essential data that informs the clinical approach to treating patients. Translating these findings from the lab to the clinic is paramount, particularly in exploring potential treatment opportunities that could redefine how Alzheimer’s is managed. This synergy between basic and clinical research fosters innovation and breakthroughs, ultimately enhancing patient care and outcomes.
Community Initiatives for Alzheimer’s Awareness
Community initiatives play a pivotal role in raising awareness about Alzheimer’s disease and supporting affected individuals. Organizations focused on educating the public about the importance of early detection and intervention deliver resources and foster dialogue surrounding neurodegenerative diseases. Such initiatives not only inform families about the signs of Alzheimer’s but also encourage engagement with ongoing research priorities, including studies centered on microglial function.
Advocating for public education on Alzheimer’s can also influence funding and research priorities, ensuring that vital resources continue to flow into the exploration of treatments for this disease. Support groups, mental health programs, and community outreach enrich the lives of those affected and facilitate a more profound understanding of the challenges presented by Alzheimer’s. As awareness continues to grow, the collective effort in combating this condition becomes increasingly formidable.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are essential components of the brain’s immune system and play a pivotal role in Alzheimer’s research. They help clear out damaged cells and prune synapses, processes that, when disrupted, can contribute to neurodegenerative diseases like Alzheimer’s. Understanding microglial function can lead to new therapeutic strategies to combat Alzheimer’s disease.
How does Beth Stevens’ research impact treatment for Alzheimer’s disease?
Beth Stevens’ research has revolutionized our understanding of microglial cells and their role in Alzheimer’s disease. Her findings highlight how aberrant synaptic pruning by microglia can lead to neurodegenerative diseases. This research provides a foundation for developing new treatments and identifying biomarkers for early detection of Alzheimer’s.
In what ways does the brain’s immune system influence Alzheimer’s progression?
The brain’s immune system, primarily mediated by microglial cells, influences the progression of Alzheimer’s disease by maintaining synaptic health and clearing debris. Dysfunctional immune responses can lead to excessive pruning of synapses, contributing to cognitive decline observed in Alzheimer’s patients. Continued research in this area is crucial for developing effective treatment approaches.
Why is microglial research important for understanding neurodegenerative diseases?
Microglial research is vital for understanding neurodegenerative diseases because these cells are central to the brain’s immune response and homeostasis. Aberrant microglial activity has been linked to various disorders, including Alzheimer’s disease. By studying microglial functions, researchers like Beth Stevens aim to uncover mechanisms that could lead to innovative treatments for these debilitating conditions.
What are the implications of Beth Stevens’ work on Alzheimer’s biomarkers?
Beth Stevens’ work on microglial cells and synaptic pruning has significant implications for Alzheimer’s biomarkers. Her research could lead to the identification of new biomarkers that detect neurodegenerative processes earlier, which is crucial for timely interventions and better patient outcomes in Alzheimer’s disease.
How might future Alzheimer’s treatments be influenced by research on microglial cells?
Future Alzheimer’s treatments may be profoundly influenced by research on microglial cells, as understanding their role in synaptic pruning and immune responses could reveal new therapeutic targets. By addressing the dysfunctional activity of microglia, researchers aim to develop drugs that can modify disease progression and improve the quality of life for patients.
| Key Points |
|---|
| Beth Stevens’ research focuses on microglial cells and their role in Alzheimer’s disease. |
| Microglia act as the brain’s immune system, clearing away damaged cells and pruning synapses. |
| Aberrant pruning by microglia is linked to Alzheimer’s, Huntington’s disease, and other disorders. |
| Stevens’ work aims to develop new medicines and biomarkers for early detection of neurodegenerative diseases. |
| An estimated 7 million Americans live with Alzheimer’s, and the number is projected to double by 2050. |
| Stevens emphasizes the importance of basic and curiosity-driven science for advancing medical research. |
Summary
Alzheimer’s research is crucial as it explores the complexities of neurodegenerative diseases and the role of the brain’s immune system. The innovative work led by Beth Stevens provides invaluable insights into how microglial cells can impact the development and progression of Alzheimer’s disease. Through her research, Stevens not only highlights the challenges posed by aberrant cell behaviors but also paves the way for new therapeutic interventions that could transform the lives of millions affected by this condition.