TIM-3 therapy for Alzheimer’s is emerging as a groundbreaking approach that harnesses the immune system’s potential to fight this devastating disease. Recent research indicates that by targeting TIM-3, a checkpoint molecule typically used to regulate immune responses in cancer therapies, we can potentially rejuvenate microglial cells in the brain. This allows these immune cells to effectively clear amyloid plaques associated with Alzheimer’s, leading to significant cognitive improvements in clinical models. Studies have shown that inhibiting TIM-3 can free up these brain immune cells to engage in plaque clearance, highlighting a novel intersection between Alzheimer’s treatment and established immune system cancer therapy. As scientists continue to explore this innovative cognitive improvement therapy, the prospects for effective Alzheimer’s solutions appear increasingly hopeful.
Recent advancements in Alzheimer’s disease research have shed light on a novel therapeutic avenue, sometimes referred to as TIM-3 blockade therapy. This cutting-edge strategy explores the use of checkpoint inhibitors traditionally employed in immune system cancer treatments, aiming to restore functionality to microglia, the brain’s resident immune cells. By effectively turning off the TIM-3 molecule, researchers have discovered a potential route for enhancing memory and cognition in Alzheimer’s patients. With the rising prevalence of Alzheimer’s, developing therapies that promote the clearance of toxic plaques while leveraging knowledge from cancer immunotherapy is more crucial than ever. The application of this innovative approach could redefine how we understand and treat cognitive decline in aging individuals.
Understanding TIM-3 Therapy for Alzheimer’s Disease
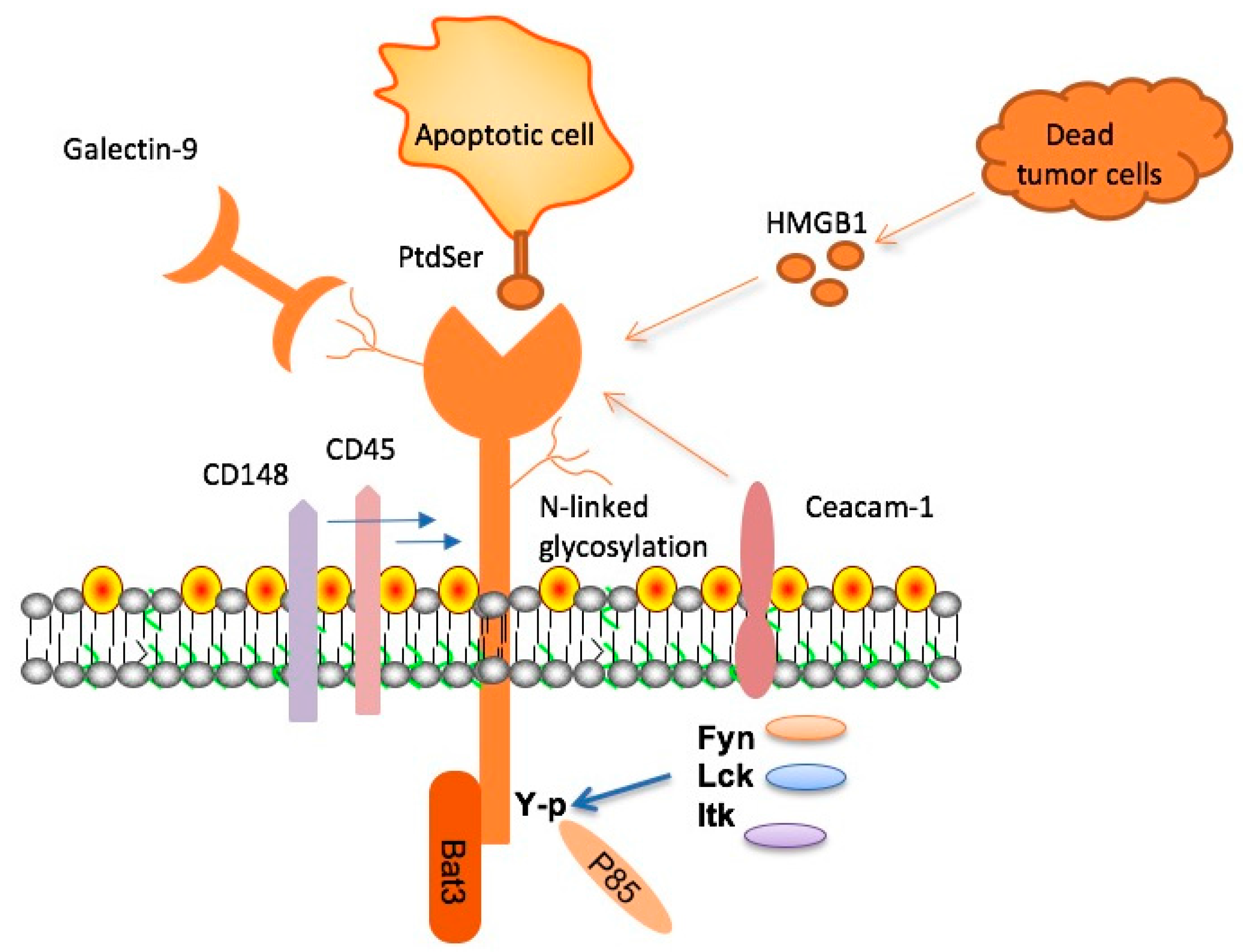
TIM-3 therapy represents a groundbreaking approach in the treatment of Alzheimer’s disease by leveraging immune system mechanisms similar to those used in cancer therapies. The TIM-3 (T-cell Immunoglobulin and Mucin Domain-3) protein has significant implications for cognitive improvement therapy as it regulates the function of microglia, the brain’s immune cells. In patients with Alzheimer’s, TIM-3 expression on microglia inhibits their ability to clear harmful amyloid plaques, which are detrimental to neural function. Recent studies have demonstrated that by targeting and blocking TIM-3, researchers can unleash these immune cells to more effectively attack and clear these plaques, potentially leading to significant cognitive enhancement in affected individuals.
Research indicates that the inhibition of TIM-3 not only facilitates the removal of toxic plaques but also enhances overall memory function. This research could revolutionize Alzheimer’s treatment by transitioning from traditional methods to more innovative immune-based therapies. Antibodies targeting TIM-3 may provide a means to restore microglial functionality, making them active players in combating Alzheimer’s pathology. As scientists continue to explore this therapeutic avenue, the hope is to develop a viable treatment option that provides a cognitive improvement therapy to mitigate the effects of Alzheimer’s and restore quality of life to patients.
The Role of Microglia in Alzheimer’s Disease
Microglia are the brain’s resident immune cells and play a crucial role in maintaining brain health. These cells are responsible for eliminating waste, including damaged neurons and protein aggregates such as amyloid plaques. In the context of Alzheimer’s disease, the dysfunction of microglia, exacerbated by high levels of TIM-3, results in an accumulation of plaques that interfere with cognitive function. By understanding the immune response in Alzheimer’s and the factors that lead to microglial dysfunction, researchers can develop targeted treatments that reactivate these vital cells. This aligns significantly with current strategies in cancer therapies where immune checkpoint inhibitors are already making a profound impact.
Research has shown that microglial activation is typically beneficial, enhancing synaptic plasticity and facilitating neuroprotection. However, in the context of Alzheimer’s, the excessive expression of checkpoint molecules like TIM-3 restricts microglia’s ability to perform these functions. Intervening with TIM-3 therapy could restore microglial activity and enhance their efficiency in plaque clearance, therefore slowing the progression of Alzheimer’s disease. This knowledge shifts the perspective on Alzheimer’s treatment, positioning it alongside advances seen in immune system cancer therapy.
Investigating Checkpoint Inhibitors and Alzheimer’s Disease
Checkpoint inhibitors, extensively used in cancer treatment, have emerged as a promising area of exploration in Alzheimer’s research. By modulating the immune system’s response, these inhibitors can potentially reverse the microglial suppression caused by molecules such as TIM-3. The dual role of TIM-3 in both cancer and Alzheimer’s creates an intriguing intersection, suggesting that therapies developed for one condition may be beneficial in the other. This approach opens avenues for cognitive improvement therapies that could mitigate plaque accumulation in Alzheimer’s disease, much like they inhibit tumor growth in cancer patients.
Aligning the strategies seen in immune system cancer therapy with Alzheimer’s treatment could provide a significant breakthrough. The successful application of checkpoint inhibitors in oncology showcases the potential efficacy of applying similar methodologies to neurodegenerative diseases. Current studies focus on understanding how TIM-3 antagonists could promote microglial activity in Alzheimer’s, enabling the clearance of amyloid-beta plaques and potentially slowing cognitive decline. By prioritizing this research, we may uncover new therapeutic strategies that harness the power of the immune system to combat Alzheimer’s disease effectively.
Challenges of Traditional Alzheimer’s Treatments
The landscape of Alzheimer’s treatment has long been dominated by approaches targeting amyloid-beta plaques directly, with mixed success. Traditional treatments have often led to limited cognitive improvement, revealing the need for innovative strategies that address the underlying mechanisms of the disease. One significant challenge is that a substantial amount of amyloid-beta does not just exist in the brain but also in the vascular endothelium, complicating the efficacy of antibody therapies. Many anti-amyloid treatments have been associated with adverse effects, including the risk of stroke due to vascular damage.
Given these challenges, the emerging TIM-3 therapy offers a refreshing perspective by shifting the focus from merely removing plaques to enhancing the body’s existing immune response. By targeting immune checkpoint molecules, researchers are exploring ways to harness the microglial cells’ natural functions to restore cognitive capabilities without the adverse side effects associated with traditional Alzheimer’s medications. This innovative approach could pave the way for a new class of therapies that address both cognitive decline and the underlying pathological features of Alzheimer’s.
The Future of Alzheimer’s Treatment with TIM-3 Antibodies
As research into TIM-3 therapy for Alzheimer’s disease continues to evolve, the potential for impactful intervention grows. Researchers are currently examining how existing anti-TIM-3 antibodies can be repurposed to treat Alzheimer’s effectively. The ability to target the specific molecular pathways that hinder microglial function opens doors for creating therapies that can drastically change the Alzheimer’s treatment paradigm. The prospect of using TIM-3 inhibitors not only highlights the symbiotic relationship between the immune system and neurodegeneration but also underscores the broader potential of immune targeting in brain diseases.
Future clinical trials will be crucial for determining the efficacy and safety of TIM-3 antibodies in human patients. By advancing our understanding of this molecular target, we move closer to uncovering viable treatment options that may prevent or delay the onset of cognitive decline attributed to Alzheimer’s. This trajectory of research highlights the importance of continued investigation into the immune mechanisms underpinning Alzheimer’s disease and how they can be leveraged for therapeutic development.
Microglial Function and Memory Preservation
Microglia play a fundamental role not just in the immune response but also in the maintenance of healthy neural circuits. They are responsible for the pruning of synapses during development, ensuring the brain retains the most relevant connections for memory formation and storage. In the context of Alzheimer’s disease, the maladaptive activation of microglia can inhibit memory preservation. By understanding how TIM-3 expression shifts microglial function, researchers aim to devise strategies to enhance synaptic health and memory retention in individuals at risk or already suffering from Alzheimer’s.
The restoration of proper microglial function through TIM-3 blockade presents a novel avenue for interventions aimed at promoting cognitive stability. If microglia can be trained or induced to resume their role in clearing amyloid plaques while preserving essential synaptic connections, patients could experience not just a slowing of cognitive decline, but restoration of lost cognitive functions. This approach emphasizes the necessity for innovative therapies that are not only focused on clearing harmful substances but also on sustaining the brain’s inherent abilities to learn and remember.
Potential for Cognition Restoration with TIM-3 Inhibition
Inhibition of TIM-3 may provide a groundbreaking therapy for cognition restoration in Alzheimer’s disease patients. By freeing microglia to perform their natural function of clearing amyloid plaques, we have an opportunity to revive lost cognitive capabilities. Empowering these immune cells to effectively combat the accumulation of beta-amyloid protein represents a shift towards restoring cognitive function, rather than just slowing deterioration. Preliminary studies in mice have demonstrated promising results, where cognitive improvement has been observed following TIM-3 gene deletion.
This innovative direction in Alzheimer’s treatment underscores the importance of understanding the complex relationship between immune response and neurodegeneration. As the research progresses, the hope is to translate these findings into human studies that could lead to effective TIM-3 therapies. If successful, this strategy could not only change the way we understand Alzheimer’s pathology but also fundamentally reshape treatment approaches to focus on restoration and enhancement of cognitive functions.
Next Steps in TIM-3 Therapy for Alzheimer’s Research
Moving forward, the future of TIM-3 therapy for Alzheimer’s disease hinges on expanding clinical research and collaboration among different scientific disciplines. Ongoing studies aim to determine the effectiveness of TIM-3 antibody therapies tested in mouse models that more accurately reflect human Alzheimer’s pathology. Establishing a robust pipeline for these therapies will be vital as researchers work to confirm their safety and therapeutic harmony in human subjects, making it a daunting yet exciting frontier in Alzheimer’s treatment.
Moreover, the collaboration between researchers, clinicians, and pharmaceutical entities will be essential to the rapid advancement of TIM-3 therapies. Continued funding and support from institutions like the National Institutes of Health are crucial for pushing these studies forward. Through this rigorous scientific inquiry, the potential for innovative Alzheimer’s treatments that leverage the immune system’s power remains a promising avenue that could yield transformative results for patients suffering from this devastating disease.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s focuses on inhibiting the TIM-3 checkpoint molecule, which normally suppresses microglia, the immune cells in the brain, preventing them from clearing amyloid plaques. By using anti-TIM-3 antibodies or small molecules, this therapy aims to enhance the activity of microglia to clear these plaques and potentially improve cognitive function in Alzheimer’s patients.
How does TIM-3 relate to Alzheimer’s treatment and immune system function?
TIM-3 is an inhibitory checkpoint molecule that regulates the immune response in the brain. In Alzheimer’s treatment, targeting TIM-3 can reverse its inhibitory effects, allowing microglia to effectively clear amyloid-beta plaques. This approach reflects a novel use of immune system strategies, traditionally used in cancer therapy, for neurodegenerative diseases like Alzheimer’s.
Can TIM-3 therapy lead to cognitive improvement in Alzheimer’s patients?
Research indicates that TIM-3 therapy may lead to cognitive improvement by freeing microglia to clear harmful plaques in the brain. In mouse models of Alzheimer’s disease, inhibiting TIM-3 resulted in reduced plaque accumulation and improved memory performance, suggesting a potential for similar outcomes in human Alzheimer’s treatment.
What role do microglia play in TIM-3 therapy for Alzheimer’s?
Microglia are the brain’s immune cells responsible for clearing debris, including amyloid plaques associated with Alzheimer’s disease. TIM-3 therapy enhances microglial activity by inhibiting the TIM-3 checkpoint, allowing these cells to attack and remove plaques, which could restore cognitive function.
What are the implications of TIM-3 being a genetic risk factor for Alzheimer’s?
The association of TIM-3 with late-onset Alzheimer’s as a genetic risk factor underscores its potential as a therapeutic target. Understanding this link allows researchers to explore how TIM-3 modulation could not only treat existing Alzheimer’s disease but also potentially prevent its onset in genetically predisposed individuals.
What types of clinical studies are being conducted for TIM-3 therapy in Alzheimer’s?
Current studies include trials using human anti-TIM-3 antibodies in mouse models of Alzheimer’s to evaluate their effectiveness in halting plaque development. This research aims to gather data on the safety and efficacy of TIM-3 therapy, paving the way for future clinical trials in humans.
What are the challenges of developing TIM-3 therapy for Alzheimer’s?
Challenges include ensuring the selective targeting of TIM-3 in the brain without affecting other systems, as well as confirming efficacy in human trials after promising results in animal models. The complexity of Alzheimer’s pathology also necessitates careful investigation into long-term effects and possible side effects of TIM-3 inhibition.
| Key Point | Description |
|---|---|
| Study Overview | Research indicates that TIM-3 therapy could improve cognitive function in Alzheimer’s by enhancing microglial activity. |
| Role of TIM-3 | TIM-3 is an immune checkpoint molecule that prevents microglia from clearing harmful plaques in the brain. |
| Microglia Function | Microglia are crucial for clearing plaques and maintaining synaptic health, but TIM-3 hinders their function in Alzheimer’s. |
| Animal Study Results | TIM-3 genetically deleted mice showed improved memory and reduced plaque burden after microglial activity was enhanced. |
| Potential Therapy | Anti-TIM-3 antibodies or small molecules may be utilized to block TIM-3’s inhibitory effects in Alzheimer’s treatments. |
| Future Research | Ongoing studies aim to evaluate human anti-TIM-3’s effectiveness in preventing plaque development in Alzheimer’s models. |
Summary
TIM-3 therapy for Alzheimer’s represents a promising frontier in the fight against this debilitating disease. By blocking the TIM-3 checkpoint molecule, researchers hope to unleash microglia’s ability to clear toxic plaques from the brain, significantly improving cognitive function. Current studies suggest that this approach not only reduces plaque accumulation but may also enhance memory performance, offering new hope where traditional therapies have failed. As clinical trials progress, TIM-3 therapy may transform Alzheimer’s treatment, paving the way for effective intervention in late-onset cases.